Psychiatric hospitals are institutions that are often frightening for lay people, because they incarnate madness and spur the imagination. They are also institutions that – perhaps even more than prisons – represent imprisonment and dispossession of the self. In an interview in the late 2000s, one young man, a former delinquent who lived in a public housing development, confided to me, “The cops, the worst thing they can do to us is to send us to psychiatry. Prison is nothing compared to that. I’ve seen guys leave psychiatry and they were vegetables”. Whether in everyday or intellectual discourse, speaking of psychiatry is also evoking psychiatric power and its potential excesses.
“Psych” power: from the denunciations of the 1970s to contemporary analyses
A widespread movement in the 1960s and 1970s denounced the social control exerted by institutions as well as psychiatric professionals, as the anti-psychiatric movement attests. The movement paid particular attention to the power that care providers exercise over patients, considering psychiatrists to be accomplices of state domination. They serve to maintain the social order, and their power resides in a knowledge whose legitimacy was first established in the nineteenth century.
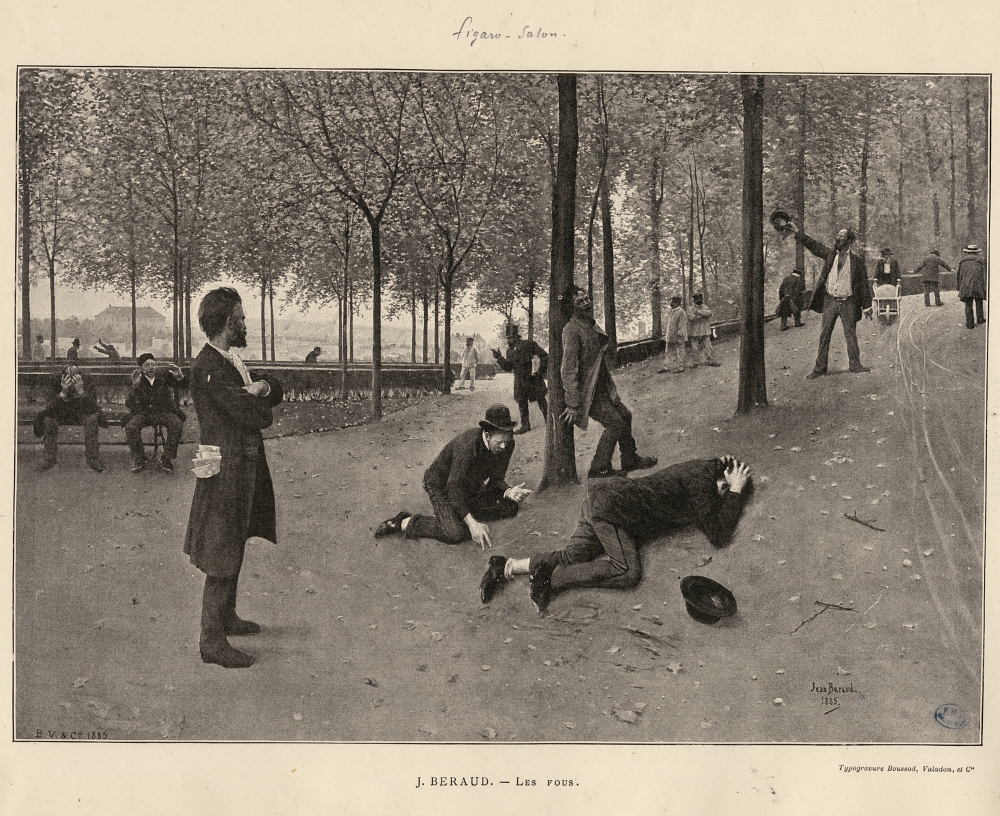
Les Fous, Jean Béraud, engraving (1885)
The writings of Erving Goffman, Robert Castel, and Michel Foucault could have been read from this perspective at the time. The expanding mandate of mentally oriented “psych” disciplines and the spread of associated forms of knowledge throughout society were furthermore challenged in analyses speaking in terms of the “psychologization”, “medicalization”, and “psychiatrization” of social issues, this expansion being judged partly responsible for the depoliticization of social relations 1.
San Clemente, Raymond Depardon, 1982.
But in the 1970s, the sub-disciplines of the sociology of professions and the anthropology of health in Anglophone countries began to make less generalizing analyses of medical power. They depicted the medical order as a “negotiated order”, this negotiation taking place both within medical teams of a variety of professional statuses, and between these providers and patients. Some dimensions of Foucault’s work that had been little used in France experienced more immediate posterity in these analyses, which pursued his thoughts on how institutions not only subjectify us, but “subjectivize” us as well as, thus contributing to making us into a certain type of subject.
Urban Portrait of Michel Foucault.
Nikolas Rose pursues this avenue paved by Foucault in his 1989 book, Governing the Soul: The Shaping of the Private Self. He defends the idea that mentally oriented disciplines play a key role in shaping “governable subjects”, based in an authority that is compatible with the principles of liberalism and democracy. In the process, he explores techniques of intervention (“human technologies”) developed in the twentieth century in several fields, including government, the military and civilians in wartime, the regulation of enterprise, and forms of early childhood intervention. He does not depict “psych-” power as a simple hierarchical domination that crushes subjectivities; for that matter, “subjectivity” only exists under the governmental techniques that give it form. For Rose, it is a power allowing individuals to bear the weight of their freedom in a society that, due to its foundational values of independence and self-realization, forces them to be free in that sense of the term2. The critical approach adopted by Rose is thus different from that taken by theories of social control.
In her lengthy contemporaneous ethnographic study in an emergency psychiatric unit in the United States, Lorna Rhodes situated her work even more explicitly in the pursuit of renewing Foucauldian thought. Power is not limited to a few individuals or groups, nor is it only vertical (the state over providers, doctors over patients): it is “fluid and diffuse, operating in a net-like grid of relationships”. In the introduction to Emptying Beds, Rhodes’ book on the study that was published in 1991, she wrote: “The staff did not employ a single kind of power. Nor did they use their powers in a clear unidirectional way”3. She also noted that the knowledge upon which this power is built is a knowledge produced by “bricoleurs”, mixing various presumably competing theories in the intellectual field, used in turn according to their potential practical utility: “At any moment, and sometimes all in the same moment, a staff member might be a biological empirist, a Freudian, or a Laingian antipsychiatrist”4. The care staff is bound together by the need to act despite the contradictions and dilemmas that fill their daily life – they have to care for patients “in crisis” that no-one wants, treat them as well as possible, respect their rights, and “empty beds” rapidly. Care professionals are aware of these contradictions and prove to be open to the presence of an ethnographer, hoping that she will reconfigure the puzzle in which they work: “You are the listener. People use you as a bridge, to feel connected to each other… we [each] have something to say [to you] which is part of the puzzle”5.
Since the early 2000s, these issues have received renewed attention from French researchers, and ethnographic research on psychiatric institutions from such approaches has experienced a relatively late boom among French sociologists7. The distancing from theories of social control is partly due to transformations occurring within psychiatric institutions as a result of the de-institutionalization process, how the sector is implanted (bringing sites of care closer to places of residence with psychological care centers [Centre médico-psychologique; CMP]), and the increasing formalization of patients’ rights. While not denying the existence of medical domination, these studies draw attention to care professionals’ reflexivity. While revealing what constraints are included in interventions, they also explore how care is intended to increase patient autonomy (i.e., their ability to live alone outside of the hospital) and question the forms of regulation that guide professional practices.
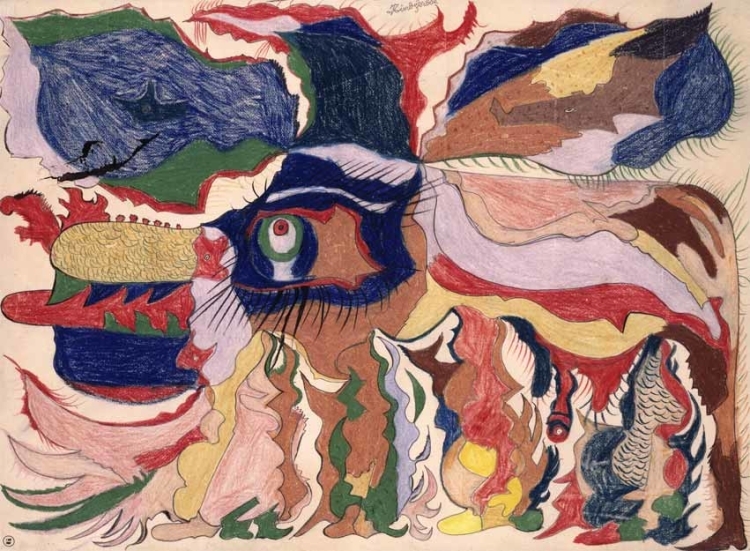
Gaston Duf, Rinôcêrôse, 1950, colouring pencils on paper 50 x 68 cm, Collection de l'Art Brut, Lausanne.
Treating adolescents’ behavioral problems: Abusive psychiatrization?
In continuity with the aforementioned work, my research trajectory led me to consider psychiatric power as jointly constructed, within care teams and between them and patients and/or their families. Although I was particularly interested in psychiatric care for “behavioral problems” in working-class youth, I was first led to emphasize the vagaries of what might appear to be an excessive medicalization of social issues. Certain adolescent behaviors that are highly regarded in street culture (keeping your guard up, defending your honor, refusing public situations of subordination) seemed to me to be arbitrarily pathologized. What institutions considered “abnormal” could indeed be “normal” according to the norms of street culture. For instance, one girl said that she did not understand why the youth counselors and “shrink” made her talk about her early childhood and her parents’ separation in order to make sense of her violence, when this very violence had been a way for her to earn respect in her neighborhood. She had moved there from a neighboring village and was first treated like a “clown”; with no brother or father to defend and protect her from the blows of other teens, she had to learn “to be the aggressor rather than the victim”. To her thinking, her violence came more from social causes than psychological ones. Her explanation corroborated analyses indicating an excessive psychologization of juvenile deviance8.
My analyses became more complex with a study I conducted late in the first decade of the 2000s in a psychiatric unit in an underprivileged area on the outskirts of Paris, which was focused on the treatment of adolescent “behavioral problems” – in this case primarily concerning youth from the insecure working classes9. This complexity is partly due to the fact that the category “behavioral problems” refers to a wide range of psycho-pathological profiles that may be more or less debilitating in terms of interpersonal relations and the possibilities for living as a functional member of society. Some of the young people in care seemed much like the young people one finds in group homes, while it is difficult to engage with and maintain a conversation with others. Although analyzing “behavioral problem” interventions in the register of excessive psychologization is challenging, it is significant that care-professional teams, led by psychiatrists, denounce the potential instrumentalization of psychiatry by youth, social, and legal services themselves. When a youth home director requested a “difficult” teenager be admitted to the unit on the grounds that she needed “a place where she can be depressed”, the unit’s chief psychologist retorted, “Why do you think we’ll do better than you”? In another instance, another psychiatrist shot back, “It’s not up to us to stop kids from burning cars, that’s not our job, it’s up to the police to do that”.
“Working on the alliance”
Observations of professional practices in meetings, interviews with patients and their families, and informal interactions, and the subsequent analysis of the “indigenous” lexicon (i.e., the everyday words used by care professionals) all furthermore indicate the importance of what they call “alliance work”. Contemporary psychiatric work has the particularity of having to justify itself: since it is intended to increase patients’ autonomy to make it easier for them to participate in society, it tries to make them into partners in their own care, which presupposes managing to convince them of the validity of the decisions taken and, if possible, including them in the process. The sense of doing “good work” is largely based on having a good feeling about the “alliance” they have with patients and their families.
This may lead the team to delay the decision to hospitalize when a family is thought to be “ambivalent”. In the case of one girl who I first met in pediatrics following her attempted suicide by drinking bleach following family conflict (she was only twelve and a half at the time), the possibility of psychiatric care in a day clinic was raised regularly with her mother over several long months without success, despite the degradation of the situation (behavioral problems, dropping out of school, “risky behaviors”, delinquent acts). The adolescent lived with her mother (a hospital service employee) and an older brother and sister (her parents had separated when she was one year old). The care team heard nothing of her for a year, until she was once again hospitalized in pediatrics after another suicide attempt by medications at age 14. In the mean time, she had been placed in a foster home by court order, and had run away. The psychiatrist who visited her in the emergency room saw her clinical situation as worsening, adding “near prostitution” to the list of previous observations in her file.
This time the mother agreed to have her daughter taken into psychiatric care for an evaluation of her condition, but quickly expresses reservations, mainly about the medications that she was being given. Someone in the care team suggested asking a judge for a court-ordered commitment (“ordonnance de placement provisoire à l’hôpital”; OPP) in case the mother should decide to check her out against medical advice. The unit chief refused to consider it without discussing it with the mother first, believing that there was “an ethical question” and, since the “alliance” with the mother was “fragile”, that they had to take care not to “break” it. Moreover, since the girl was hostile to the idea of a placement in supervision prior to admission, one of the psychiatrists recommended a compromise:
It’s ridiculous to force a kid to go someplace else, they’ll run away. But we have to support and re-introduce the father, so there’ll be a third party between the mother and the daughter. We have to work on the separation of mother and daughter, but without rushing.
The “right way of doing things” that emerges from various episodes of her care is structured by ethical issues and criteria for therapeutic effectiveness. For psychiatrists, it is a matter of not overstepping their role or destroying their prior work. This concern, which amounts to being wary of the abuse of psychiatric power, probably arises from the characteristics of the unit being studied, deeply saturated as it was with the values underlying institutional psychiatry. This conception of psychiatry was fuelled by psychoanalysis, which was behind the policies in the sector in the 1960s and 1970s. While it does recognize the potential virtues of hospitalization, it was developed in opposition to asylums, which it accuses of making patients’ conditions chronic10.
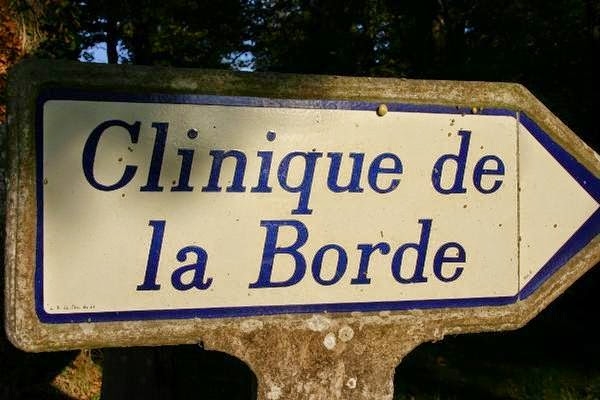
The la Borde clinic was created in 1953 by Jean Oury, promotor of the Institutional psychiatry.
The la Borde clinic, seen in 1995 by Nicolas Philibert in his movie, La Moindre des choses.
In addition to the particularities of this unit, this conception of “good work” is nonetheless part of a more general movement transforming the social state, which for both moral and economic reasons invites its agents to “work with,” and no longer “on,” their publics11. From this perspective, speech has a major role in care. At the same time, therapeutic work relies not only on restraint (detention, medical treatment) but also on the “pedagogy of reflexivity”. Whether in everyday informal interactions with front-line care providers in the unit (nurses, counselors, nurses’ aids, service employees) or in interviews with the higher-ranking care professionals (psychologists, psychiatrists, social workers) that see them only in formal settings, adolescents are led to comment on certain words or acts after the fact. They are encouraged to verbalize their feelings, which initially happens by care professionals naming the emotions they suppose the youth are feeling: In the care logbook one can read sentences such as “I verbalized his disappointment for him” and “I told him he had the right to be angry, but not to smash everything”. Adolescents gradually learn to relate to themselves in a particular way. The formal interviews come to symbolize the private, intimate space: one cannot say everything anywhere or any time (“You’ll talk about that in your interview”, care professionals sometimes remind youths in joint “provider-patient” meetings, when one of them says something that providers think is “too personal”).

Graffiti, Tabacalera in Madrid.
The moral division of labor, and the social division of labor
Faced with remonstrations from patients about how the unit operates in general or clashes with some providers, care professionals sometimes have to justify themselves. They may acknowledge the legitimacy of some demands – “we aren’t always right,” said one nurse’s aid, “we can be wrong”; “I do like everyone else – when I get insulted, I put [them] in [their] room” confided a counselor, “but that might not be the only solution”. Sometimes, however, front-line care providers, who have to deal with adolescents in the in-patient unit every day, condemn the “laxity” of the psychologists and psychiatrists, who only see them in a formal setting. Care providers on “the second floor” (the closed in-patient unit), who are in physical proximity to the patients, regularly set themselves apart from those on “the first floor” (which contains only offices: psychologists and psychiatrists, the pediatrician, the manager, the secretaries, and a social worker). A nurse’s aid that was the victim of a physical attack explains:
When a young person attacks you, they [the psychiatrists and psychologists] tell you that it’s not you, the person that they attacked, that they are attacking the institution. But in the mean time your body is still part of you! The skin, hair, the emotion, you can’t put them aside saying you can’t pay it any heed because it’s the setting and the institution. (…) The doctors are often criticized for the lack of return on acts caused by the young people. Or, we should have an explanation so we can understand. Sometimes I have the impression that the psychiatrists don’t want to have the bad guy role in the work they do with the young people, they can’t allow themselves to do certain things. Repression is lacking a little bit. I think that sometimes it’s necessary to impose sanctions. Being sick doesn’t exclude sanction. It would make it possible for care providers to feel more supported.
This remark was particularly aimed at one psychiatrist who is heavily influenced by psychoanalysis and quite vigilant over the proper treatment of adolescents, who always presses care providers to think about their role in setting off incidents. The moral division of labor (what each considers to be “good treatment”) is thus related to the social division of labor (the tasks each performs according to his or her place in the unit hierarchy). The psychiatrist in charge of the unit must thus ultimately reach decisions by arbitrating between what he thinks he owes to patients and the complaints of front-line care providers, since the stability of his team (minimizing turn-over and absenteeism) is also an essential condition for good treatment.

Manie de la persécution du Pierrot, Paul Klee, 1924, Centre Pompidou.
Transmitting a “power to speak”
As is common practice in ethnography, I kept a daily field journal for the nine months of field research, during which I spent an average of three days per week in the unit. Re-reading this journal prompted me to try to understand what care providers meant when they used recurring expressions such as “working on the alliance”, “working on family relations,” “working with the running away” (or other troubling situation), and “working upstream”. This re-reading also made me aware of one essential criterion for evaluating “good work”: the psychologists and psychiatrists are satisfied with the work they have done when an adolescent “was able to say” something that they considered to be important, because it is the first time that he or she has shared it or because it is expressed with apparently genuine emotion.
Daniel was put into in-patient care at age 12 for suicide risk, and had also been oriented to a youth home (Institut Thérapeutique Educatif et Pédagogique; ITEP) for behavioral problems, agitation, and difficulties in concentration. As a baby children’s services had placed him with a home-based childcare provider because his mother, a minor and undocumented immigrant from the Congo, was unable to find a place in a mother-and-children’s shelter. For a long time the mother lived in insecurity and could not maintain regular contact with her child. When Daniel was six he was placed in a children’s home because his care provider suffered a stroke and was unable to look after him anymore. His mother, whose situation had stabilized and who had had other children in the intervening time, was thought to be ambivalent toward her son, who was already manifesting problems, so social services decided to keep him in foster care. Relations between the mother and social services continued to degrade, and by the time Daniel was admitted to the unit he had not seen his mother for three years. One of the goals of care was to renew these ties. Before the reunion, Daniel expressed a mix of joy and apprehension (“I’m happy” / “I’m afraid”); a few hours afterward he confided to his psychologist that his mother had been “moved” by it. Describing how Daniel’s therapy had progressed to the rest of the team, the psychologist remarked, “I am happy that he was able to say that, that he was able to use these very words”. The transmission of a “power to speak” to patients is an integral part of psychiatric power in its contemporary form.
Fatima, a chronicle of reconstruction
The path taken by Fatima, who was born in the Parisian metropolitan area in 1984, is emblematic of the dual process of subjection and subjectivation – of self-construction – that may occur under care, and of the ways in which interventions can take on meaning for patients. When I met her, in 2001, she was just short of 17 years old12. She had an internship in an integration program of the legal youth protection services (Protection Judiciaire de la Jeunesse) and was working on an activities coordinator certificate (“brevet d’aptitude aux fonctions d’animateur”; BAFA). The previous year she had spent six months in a psychiatric unit for adolescents after living eight months as a runaway following violent family conflict. Her parents, who were originally from Morocco, were worried about respectability and had been overwhelmed by their youngest daughter’s demands and activities. She had gotten “caught up in” delinquency, unlike their other children. She answered their rigidity with ever more deviance, and the relationship degenerated: after being detained for extortion, her father and brothers beat her then tied her up and left her overnight in the cellar, until she was freed by her sister-in-law.
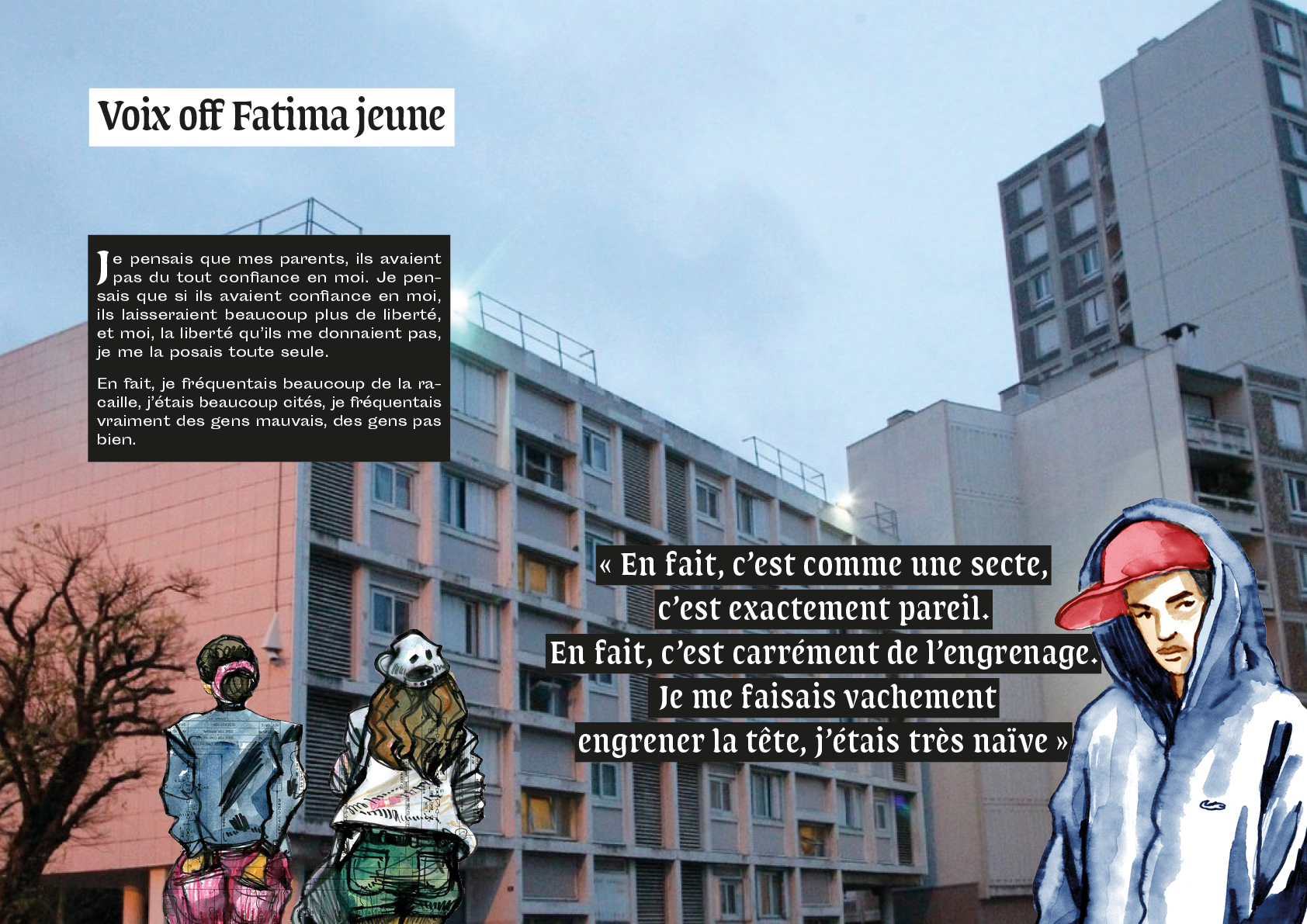
Extract of the movie project: Fatima, chronique d'une reconstruction, by Isabelle Coutant and Marie Maffre ; drawings Damien Roudeau ; graphic design Guillaume Lavezzari.
When we first met, Fatima spoke at length about “her” psychiatrist in glowing terms. But when she was first admitted to the hospital she had refused any relationship with him, facing him mutely. He was able to convince her to tell her story in writing, with a nurse’s help. He was gradually able to loosen her reserve, and bit by bit, during family interviews, managed to rebuild ties between Fatima and her parents as a prelude to a return home. Fatima explained after the fact that she had been “lost” and that the psychiatrist had helped her to find her “old self”: her time in care had put an end to the seemingly endless spiral, breaking away from relationships she’d developed in the “street”. She thought that she would not have been able to do it without support, because she was attached to the people that had taken her in during the long hard months, and she could not have managed to “think without them”. She emphasized the role that he had played in rebuilding connections between her and her family, bringing each to understand the other’s perspective.

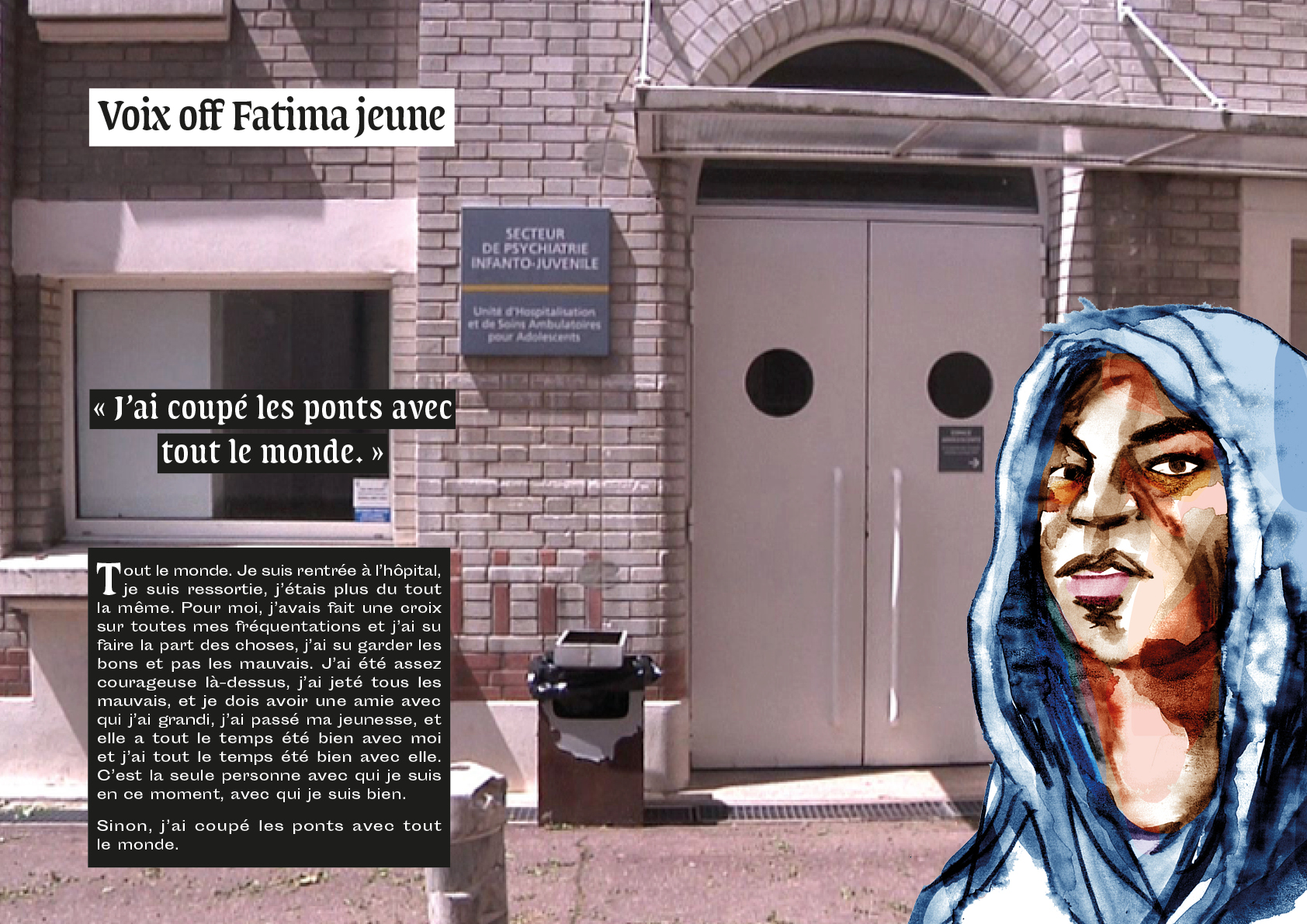
Extract of the movie project: Fatima, chronique d'une reconstruction, by Isabelle Coutant and Marie Maffre ; drawings Damien Roudeau ; graphic design Guillaume Lavezzari.
Although Fatima’s discourse attests to the interiorization of psychiatric discourse, it is also the mark of years of “self-transformation work13 » – or self-cultivation. She did not need to resort to institutionalization again, but she knew she could consult a psychiatrist again at critical times: the first time she was a 21-year-old new mother in a mother-child shelter, and she sought out her psychiatrist after a violent conflict with the child’s father. The shelter staff had threatened to evict her, warning her of the consequences of this relationship that they deemed to be toxic for the child. The psychiatrist was able to reassure her that she was able to handle the situation, which helped her considerably. Years later, socially and professionally integrated (as a sales clerk in a children’s goods store) but deeply shaken by the accidental death of her sister, she went to a CMP of her own volition to consult with a psychologist for a while. Later, at age 30 and married to a sales manager 15 years her senior, she was thinking about revisiting her whole life course as part of a documentary film project. “When you talk about your youthful transgressions, it proves that you have made progress, and that you are still making progress”, she confided. As part of this project, she wanted to return to the unit to consult her medical files, out of what was probably a desire to re-open the book to better turn the page, to try to come to terms with a past that she was still ashamed of and unable to admit to her children, and to finish rebuilding herself by starting to share her story with adolescents that might see themselves in it.
Fatima, chronique d'une reconstruction, project by Isabelle Coutant and Marie Maffre ; drawings Damien Roudeau.
The psychiatric institution: A place of constraint and socialization
In addition to their restrictive dimension, psychiatric institutions are places of socialization, like all institutions. They teach a certain way of relating to oneself, and a way of managing emotions that is more compatible with dominant social norms. Some adolescents thus explain that they “learned to step away to calm down”, to speak instead of punching the wall, to ask to leave a class instead of getting agitated. For the poorest, especially those without solid family support, the hospital may even end up representing “a second family”, a refuge, which speaks volumes about their living conditions outside. After leaving, some of them ask to return, presenting the psychiatrists with a dilemma: should they respond to this request at the risk of making them chronically dependent? Can psychiatry “give asylum” without once again becoming the execrated asylum from which it sought to distinguish itself over the course of the twentieth century?
Insisting on the socializing dimension of contemporary psychiatric institutions and how psychiatric power is jointly built (including patients in the process) should not, however, lead us to oppose a discipline’s past to its very different present. This is partly because the “domestication of the dominated” by the state has always been as permeated by philanthropy as by discipline15. It is also because contemporary forms of intervention are still about discipline, although it takes another form: one that is spoken and makes speak, since this discipline is surrounded by ethical prescriptions and a certain conception of the human person, at the convergence of moral concerns and neoliberal injunctions, which muddies the waters somewhat.
But changes in power relations between academic disciplines in the field of mental health due to advances in brain imaging and cognitive sciences have partly unseated psychoanalysis and are fuelling concerns about the future of therapeutic practices attentive to “the alliance” and valuing speech as an important aspect of therapy. Professionals specialized in “behavioral problems” notably expressed their concerns in a petition (“No Zeros for Behavior”) in reaction to a 2005 report from INSERM (Institut National de la Santé et de la Recherche Médicale, the national institute for health and medical research) that recommended the early identification of “at risk” children16. Since “behavioral problems” are considered to be a risk factor for delinquency, the report’s authors cite a number of causes (social, familial, neurological, genetic) before proposing intervention in families of children from the age of three, taking the form of parental guidance, with pharmacology as a second-line treatment. Signers of the petition against this report (who were more psychoanalytically oriented) condemned the risk of early stigmatization and an excessive medicalization of social issues. In a context intensifying security issues, they are worried about the possible implementation of “training” measures, and “sedatives” should the first approach fail17.
For that matter, how can one continue to “work on the alliance” with families and adolescents if understaffing worsens? In an op-ed piece published in Libération on March 29, 2018, entitled “Child psychiatry doesn’t want to die!”, child psychiatrists Bernard Golse and Marie-Rose Moro warned of the prospects of pediatric psychiatry given the dearth of means and personnel. They note that although demand for pediatric mental care has grown significantly in the last decade, there are half as many child psychiatrists as there were ten years ago. Since the vast majority of those remaining are over 55 years old, this situation is likely to worsen if nothing is done to remedy it18.
Notes
1
Robert Castel, Jean-François Le Cerf , “Le phénomène ‘psy’ et la société française”, Le Débat, 1980, n°1, p. 32-45, n° 2, p. 39-47.
2
Nikolas Rose, Governing the Soul. The Shaping of the Private Self (Preface to the second edition), Londres, Free Association Books, 1999.
3
Lorna Rhodes, Emptying Beds, Berkeley, University of California Press, 1995, p. 6.
4
Lorna Rhodes, Emptying Beds, Berkeley, University of California Press, 1995, p. 4.
5
Lorna Rhodes, Emptying Beds, Berkeley, University of California Press, 1995, p. 3 (insertions in the original).
7
For more on the later development of the sociology of health in France, see Claudine Herzlich and Janine Pierret, “Au croisement de plusieurs mondes : la constitution de la sociologie de la santé en France (1950-1985)”, Revue française de sociologie, 51-1, 2010, p. 121-148; and for more specifically on the area of mental health, see François Sicot, “La maladie mentale, quel objet pour le sociologue ?”, Déviance et Société, 2006/2, vol. 30, p. 203-232.
8
Although the issue of the medicalization of delinquency is an old one (see especially P. Conrad, “The discovery of hyperkinesis: Notes on the medicalization of deviant behavior”, Social problems, 23, 1975, p. 12-21), it has a particular urgency in France today. For more, see Didier Fassin, Des maux indicibles. Sociologie des lieux d’écoute, Paris, La Découverte, 2004 ; François Sicot, “La psychologisation rampante de la question sociale”, in Stéphane Beaud, Joseph Confavreux, Jade Lindgaard (dir.), La France invisible, Paris, La Découverte, 2006, p. 618-631.
9
Isabelle Coutant, Troubles en psychiatrie. Enquête dans une unité pour adolescents, Paris, La Dispute, 2012 ; Isabelle Coutant “The psychiatric treatment of ‘behavioural problems’ in adolescence : between coercion and socialisation”, Anthropology & Medicine, vol. 23, 2016, p. 259-274.
10
Institutional psychiatry emerged between the two world wars, from critiques of the “asylum” form. Fuelled by psychoanalysis and experiments conducted on patients during World War II, it developed in France in the 1960s, informing policies in the sector. Although this current of thought believes in the potential virtues of in-patient care (unlike anti-psychiatry), it nonetheless denounces the attendant risks of regression and becoming chronically dependent on it. Alongside treatment by medication, speech therapies are held in particular esteem (considering the patient as a “subject”), as is the idea that the whole professional team, including the “support staff”, plays a therapeutic role.
11
Isabelle Astier, Les Nouvelles règles du social, Paris, PUF, 2007.
12
Isabelle Coutant, Délit de jeunesse. La justice face aux quartiers, Paris, La découverte, 2005.
13
This is the term that Muriel Darmon suggests when speaking of anorexics: Murielle Darmon, “The Fifth Element: Social Class and the Sociology of Anorexia”, Sociology 43-4, 2009, p. 717–33; Muriel Darmon, Becoming Anorexic: A Sociological Study (Translated by Lucy Garnier), Oxford and New York, Routledge, 2017 (2003).
15
Pierre Bourdieu, Sur l’État, Cours au Collège de France (1989-1992), Paris, Le Seuil, 2012.
16
Inserm, Troubles des conduites chez l’enfant et l’adolescent, Les Editions Inserm, Paris, 2005. The authors of the report used the definition of “behavioral problems” from the DSM, the American diagnostic manual. It declares that these problems “are expressed in children and adolescents through a range of behaviors, from flashes of anger and the repeated disobedience of the difficult child to serious attacks like rape, assault and battery, and the delinquent running away. Its main characteristic is attacking the rights of others and social norms”. The repetition and persistence of such behaviors is what leads them to be seen as “problems”. It is said to concern 3-9% of youth aged 13-18.
17
Alain Ehrenberg, “Malaise dans l’évaluation de la santé mentale”, Esprit, mai 2006, p. 89-102 ; Brigitte Chamak, “Troubles des conduites”, L’information psychiatrique, vol. 87, 2011/5, p. 383-386.
18
Libération, March 29th of 2018.
Bibliographie
Politix, Expérience et critique du monde psy, vol. 1, n° 73, 2006.
Graham Burchell, Colin Gordon, Peter Miller (eds), The Foucault Effect, Chicago, The University of Chicago Press, 1991.
Françoise Castel, Robert Castel, Anne Lovell, The Psychiatric Society (trans. A. Goldhammer) [1977], New York, Columbia University Press, 1982.
Robert Castel, The Regulation of Madness: The Origins of Incarceration in France [1977], Cambridge, Polity Press 1988.
Peter Conrad, “The discovery of hyperkinesis: notes on the medicalization of deviant behavior”, Social problems, n° 23, 1975, p. 12-21.
Isabelle Coutant, Troubles en psychiatrie. Enquête dans une unité pour adolescents, Paris, La Dispute, 2012.
Isabelle Coutant, Jean-Sébastien Eideliman, “The Moral Economy of Contemporary Working-Class Adolescence. Managing Symbolic Capital in a French public ‘Adolescent Centre’”, British Journal of Sociology, n° 64-2, 2013, p. 248-266.
Isabelle Coutant, “The psychiatric treatment of ‘behavioural problems’ in adolescence: between coercion and socialisation”, Anthropology & Medicine, vol. 23, 2016, p. 259-274.
Muriel Darmon, Becoming Anorexic: A Sociological Study [2003], Oxford and New York, Routledge, 2017.
Muriel Darmon, “The Fifth Element: Social Class and the Sociology of Anorexia”, Sociology n° 43 (4), 2009, p. 717-733.
Claude-Olivier Doron, “La contribution de Foucault au domaine de la santé mentale”, in I. Coutant, S. Wang (eds.), Santé mentale et souffrance psychique: un objet pour les sciences sociales, Paris, CNRS-éditions, 2018.
Benoît Eyraud, Livia Velpry, “Contrainte et consentement en santé mentale”, Santé mentale et souffrance psychique : un objet pour les sciences sociales, in I. Coutant, S. Wang (dir.), Santé mentale et souffrance psychique : un objet pour les sciences sociales, Paris, CNRS-éditions, à paraître.
Michel Foucault, Psychiatric Power. Lectures at Collège de France, 1973-74 [2003], New-York, Palgrave Macmillan, 2006.
Erving Goffman, Asylums: Essays on the Social Situation of Mental Patients and Other Inmates, New York, Anchor Books, 1961.
Rhodes Lorna, Emptying Beds. The Work of an Emergency Psychiatric Unit [1991], Berkeley, Los Angeles, Londres, University of California Press, 1995.
Delphine Moreau, “Après l’asile”, Labyrinthe, n° 29, 2008, p. 53-64.
Richard Rechtman, “Souffrances psychiques et évolutions de la psychiatrie”, Etudes, n° 415, 2011, p. 329-339.
Nikolas Rose, Governing the Soul. The Shaping of the Private Self [1989], Londres, Free Association Books, 1999.
Livia Velpry, Le Quotidien de la psychiatrie. Sociologie de la maladie mentale, Paris, Armand Colin, 2008.









